Encephalitis Lethargica is a neurological syndrome also known as ‘sleeping sickness’ or ‘sleepy sicknesses. The disease attack the brain, giving Parkinsonian like symptoms.
It spread across Europe and then the worldwide beginning in the winter of 1916–17, and continuing into the 1930s. A Neurologist Constantin von Economo and the pathologist Jean-Rene Cruchet described the term encephalitis lethargica in 1917. The exact number of people effected is unknown but it is estimated that more than one million people were causing directly more than 500,000 deaths. Most of the people who survived were never able to return to their normal pre-morbid vigour.
In the words of the famed neurologist and writer Oliver Sacks:
They would be conscious and aware – yet not fully awake; the patients would sit motionless and speechless all day in their chairs, totally lacking energy, impetus, initiative, motive, appetite, affect or desire; such people registered what went on about them without active attention, and with profound indifference. They neither conveyed nor felt the feeling of life; they were as insubstantial as ghosts, and as passive as zombies.

History:
In late 1916, while treating patients in, Dr Constantin von Economo found many unusual neurological symptoms while examining his patients in the Psychiatric-Neurological Clinic of the University of Vienna. He categorized patients with varying symptoms into meningitis, delirium and multiple sclerosis. However, none of them matched the exact diagnostic scheme. In 1917, Von Economo realized the uniqueness of the disease and named it Encephalitis Lethargica. A French physician, René Cruchet was confronting the same cases in a military hospital. Von Economo and Rene Cruchet wrote many articles on the particular disease. More than 9000 articles were published about perplexing disease.
There were too many factors involved in the spread of disease. In 1917, movement of troops in Europe during World War I causes the spread of encephalitis lethargica in Vienna, followed by USA and Russia in 1918. By 1919, the epidemic had occupy most of Europe, the USA, Canada, Central America, and India. Between 1920 and 1924, Peaks of epidemic were occurred. Since 20th century, there has been no epidemic recurrence of encephalitis lethargica, but putative sporadic cases continue to occur.
Sign and Symptoms:
Encephalitis lethargica was classically characterized by acute and chronic phases, although the two often blended together.
During the acute phase, patients typically presented with fever, sore throat, headache, visual abnormalities, catatonia, and sleep inversion. These symptoms could be manifested with day to day or hour by hour shifts in symptomatology. In chronic phase, patient may experience akinetic mutism or coma like stage, parkinsonian symptoms such as tremors, rigidity, muscular pains, upper body pains and behavioral changes including psychosis. The chronic phase could occur from months to years later and was most commonly characterized by parkinsonian-like signs.
Etiology:
After 100 years of pandemic the etiology of encephalitis lethargica is still erratic. Although two main categories were proposed: bacterial and viral. More recently, however, there is evidence to support a third theory: auto-immunity. It is also possible that encephalitis lethargica has multiple causes, which could explain the wide array of etiological hypotheses that have been advanced over the years.
The German neurologist Felix Stern, during pandemic examined hundreds of encephalitis lethargica patients, pointed out that their encephalitis lethargica typically evolved over time. Primary symptoms rule out sleepiness or wakefulness. Secondary symptom would lead to an oculogyric crisis. Tertiary symptom would be recovery, followed by a Parkinson-like syndrome. If patients of Stern followed this course of disease, he diagnosed them with encephalitis lethargica.
In 2010, in a substantial Oxford University Press compendium reviewing the historic and contemporary views on EL, its editor, Joel Vilensky, of the Indian University School of Medicine quotes another researcher, writing in 1930, who states, “we must confess that etiology is still obscure, the causative agent still unknown, the pathological riddle still unsolved…”, and goes on to offer the following conclusion, as of that publication date:
“Does the present volume solve the “riddle” of EL, which… has been referred to as the greatest medical mystery of the 20th century? Unfortunately, no: but inroads are certainly made here pertaining to diagnosis, pathology, and even treatment”
In 2012, Oliver Sacks in his book “Awakenings”, acknowledged about institutionalized survivors that this virus as the probable cause of the disease.
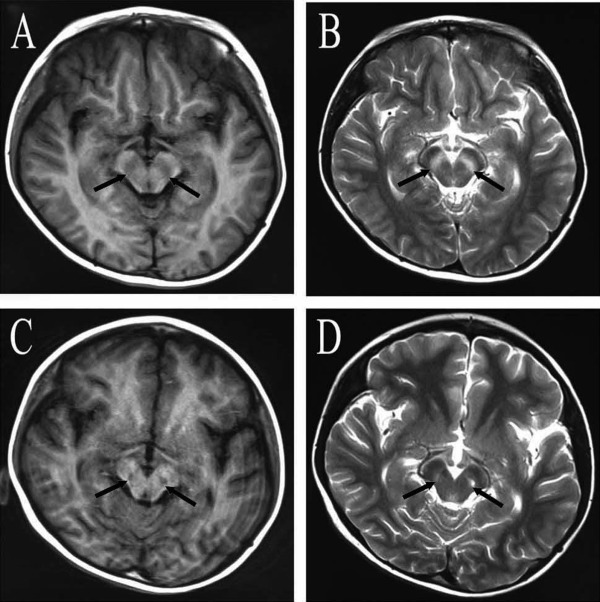
Diagnosis:
There have been many diagnostic criteria for encephalitis lethargica. The most recent diagnostic criteria suggested for encephalitis lethargica is influenza like signs hypersomnolence, wakeability, opthalomoplegia and psychiatric changes.
Treatment:
In 1929, 80 treatments were used during the epidemic but none of them were useful in this regard. Some patients were dead in their acute phase, one-third survived without sequelae, and one-third showed neurological sequelae.
However, L-Dopa (Levodopa) and anti-parkinsonism drugs were used to be very effective.
Modern treatment approaches include immunomodulating therapies.
Current State of encephalitis Lethargica:
About ~80 cases were proposed on encephalitis lethargica since 1940. However, the diagnostic criteria varies from patient to patient. At first the Von Economo’s 1929 diagnostic criteria were considered to be powerful. In 1987, Howard and Lees proposed the most recent criteria on the basis of most recent cases which involves oculogyric crisis and obsessive compulsive behavior. But no evidence were recorded in accordance to these criteria. One of the authors (J.A.V.) proposed that any diagnosis of encephalitis lethargica should be under neurological symptoms such as: (i) influenza-like prodromal signs; (ii) hypersomnolence; (iii) wakeability; (iv) ophthalmoplegia; and (v) psychiatric changes.
Vilensky concluded that only 14 reports out of 200 seemed to fit these criteria reported during 1941 to 2009. Although after 100 years of pandemic, encephalitis lethargica became a mystery without a proper diagnostic criteria behind it.
[…] Also See: Encephalitis Lethargica: Neurological Sleeping Syndrome […]